Ossification centres
With the exception of the distal femur, the ends of the long bones in the newborn are completely cartilaginous. The secondary ossification centres appear during growth in a predictable pattern (Figure 14) and knowledge of the timing and pattern of appearance is important in assessing fractures around and into the joints.
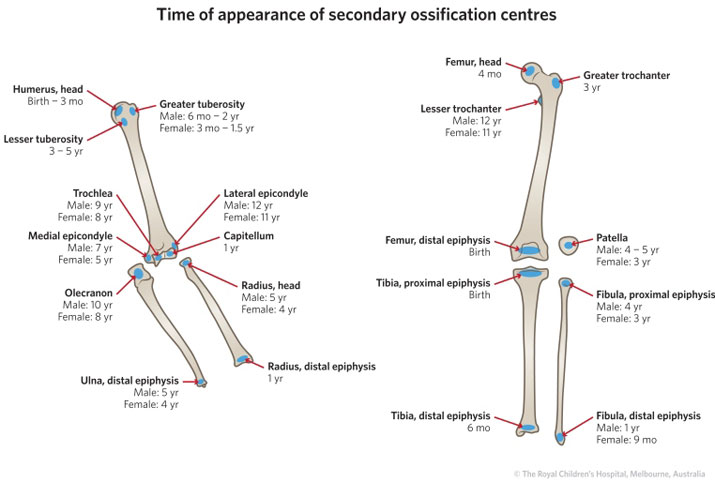
Figure 14: Typical age of appearance of the secondary ossification centres in the upper limb and lower limb.
Ossification centres of the elbow
The frequency of injury to the elbow joint in childhood demands knowledge of its cartilaginous anatomy. The distal humerus and proximal ulna and radius are completely cartilaginous at birth. The ossification centre for the capitellum develops at one year and then is followed by the radial head, medial epicondyle, trochlea, olecranon and lateral epicondyle. This order of appearance is specified in the mnemonic C-R-I-T-O-E (see Table 2).
The ages at when the ossification centres first appear is variable but the sequence remains constant. In general, the pattern of ossification occurs earlier in girls than boys. The capitellum and trochlea fuse between 10-12 years of age leaving the medial epicondyle separate until 14-17 years of age.
Progressive development of the elbow ossification centres
Table 2: Timeline of ossification centres.
| |
Age of appearance (years) |
| Ossification centre |
Girls |
Boys |
| C: |
Capitellum |
1 |
1 |
| R: |
Radial head |
4 |
5 |
| I: |
Internal or medial epicondyle |
5 |
7 |
| T: |
Trochlea |
8 |
9 |
| O: |
Olecranon |
8 |
10 |
| E: |
External or lateral epicondyle |
11 |
12 |
Injuries to the elbow may avulse a bony fragment (e.g. medial epicondyle) (Figure 15) or split major intra-articular fragments (e.g. lateral condyle) (Figure 16). Loss of normal alignment of the ossification centres may be the only indication of a more major elbow injury.
Figure 15: Medial epicondyle avulsion (red arrow). This is evident on the AP view. It is more difficult to see on the lateral view due to the splint.
Figure 16: AP and lateral view of a displaced lateral condyle fracture. The AP in this instance provides the most useful information. It shows a displaced fracture fragment. The ulna is laterally subluxated. Notice that the majority of the soft tissue swelling is located laterally and this is where the maximum tenderness is.